Paul E. Marik, MD, FACP, FCCM, FCCP; Howard L. Corwin, MD, FACP, FCCM, FCCP
Crit Care Med. 2008;36(11):3080-3084. ©2008 Lippincott Williams & Wilkins
Posted 11/05/2008
Objective: Acute lung injury (ALI) is a well known complication following the transfusion of blood products and is commonly referred to as transfusion-related acute lung injury (TRALI). The objectives of this review are to summarize current knowledge of TRALI with an emphasis on issues pertinent to the intensivist and to define the newly recognized Delayed TRALI syndrome.
Data synthesis: The classic TRALI syndrome is an uncommon condition characterized by the abrupt onset of respiratory failure within hours of the transfusion of a blood product. It is usually caused by anti-leukocyte antibodies, resolves rapidly, and has a low mortality. A single unit of packed cells or blood component product is usually implicated in initiating this syndrome. It has, however, recently been recognized that the transfusion of blood products in critically ill or injured patients increases the risk (odds ratio 2.13; 95% confidence interval 1.75-2.52) for the development of the ALI 6-72 hours after the transfusion. This delayed TRALI syndrome is common, occurring in up to 25% of critically ill patients receiving a blood transfusion, and is associated with a mortality of up to 40%. While the delayed TRALI syndrome can develop after the transfusion of a single unit, the risk increases as the number of transfused blood products increase. The management of both the classic and delayed TRALI syndromes is essentially supportive.
Conclusions: Both the classic and delayed TRALI syndromes are among the most important complications following the transfusion of blood products and are associated with significant morbidity and increased mortality. The risk and benefits of all blood products should be assessed before transfusion.
Introduction
In recent years blood transfusion requirements have been increasing because of the increasing burden of chronic disease in an aging population, improvement in life-support technology with an increasing severity of illness and blood-intensive surgical procedures.[1,2] In the United States alone, nearly 14 million units of blood are donated and 12 million units are transfused annually.[2] This increased use has occurred despite growing concern regarding the safety of blood transfusions and the benefits of a restrictive transfusion strategy.[3] These issues are particularly important in the critically ill. Two recent observational studies conducted in intensive care units’ in Europe and the United States observed that red blood cell (RBC) transfusions were administered in approximately 40% of all patients studied.[4,5] On average, critically ill patients received almost 5 units of RBCs. This has changed little over the past decade despite the scrutiny of transfusion practice.
Historically blood transfusion has been viewed as having obvious clinical benefit. However, transfusion practice has come under increased scrutiny. Initially this was driven by concerns over transfusion related infections, human immunodeficiency virus in particular. Although the risk of transfusion transmitted infections has received considerable attention,[6] it is now becoming clear that there are other important, less recognized, risks of RBC transfusion related to RBC storage effects and to immunomodulating effects of RBC transfusions in almost all recipients.[7-10] Acute respiratory distress immediately after the transfusion of blood and/or blood products has been increasingly recognized over the past two decades. This syndrome known as transfusion-related acute lung injury (TRALI), is considered the most common and serious complication associated with the transfusion of blood products.[11-13] However, it has recently been recognized that the transfusion of blood and blood products increases the risk of critically ill patients developing delayed respiratory failure. This article will review classic TRALI and the delayed TRALI syndrome.
Definitions
Respiratory complications after blood transfusion consistent with the syndrome now known as TRALI have been reported since the 1950s.[14] The syndrome has been called pulmonary hypersensitivity reaction, allergic pulmonary edema, noncardiogenic pulmonary edema, and leukoagglutin reaction. The term TRALI was initially proposed by Popovsky et al.[13] to refer to pulmonary edema complicating blood transfusion. The lack of a consensus definition of TRALI contributed to its under-recognition as a cause of lung injury. A definition emerged from the TRALI consensus conference in 2004 and from the US National Heart, Lung, and Blood Institute.[15,16] The definition was based on the widely used definition of acute lung injury (ALI) proposed by the American European Consensus Committee, which includes bilateral alveolar infiltrates, hypoxemia (Pao2/Fio2 <300 mmHg), and the clinical exclusion of cardiac failure.[17] For a diagnosis of TRALI to be made there must be no preexisting ALI before transfusion, the onset of the signs and symptoms must occur within 6 hrs of the transfusion and there must be no temporal relationship to alternative risk factors for ALI.
TRALI is therefore a distinct clinical syndrome characterized by the acute onset of respiratory distress in a patient receiving a transfusion of blood products. Symptoms include the sudden onset of dyspnea and tachypnea which typically develop within 1-2 hrs after initiation of a transfusion.[18-20] Most commonly, a single unit of blood or blood product is implicated in causing the syndrome. Patients with classic TRALI should not have other risk factors for ALI and, thus, the transfusion is the only identifiable cause of the respiratory failure.
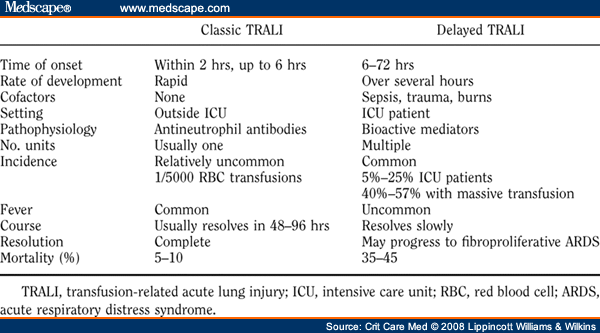
Massive blood transfusion (transfusion of one or more blood volumes or >15 units of RBC within a 24-hr period) has long been known to be a risk factor for the development of ALI/acute respiratory distress syndrome (ARDS) which typically develops many hours after the transfusions.[21-26] These patients usually have other risk factors for ARDS and do not meet the current definition for TRALI. More recent data suggest that transfusion of lesser amounts of blood and or blood products increases the risk of critically ill and injured patients developing delayed ARDS, 6-72 hrs after the transfusion of blood or blood products.[27-32] This delayed TRALI syndrome is distinct from the classic TRALI syndrome. This distinction is important, as although undoubtedly there is some overlap between the two syndromes, the pathophysiology, clinical presentation, disease progression, clinical implications, and prognosis differ considerably ( Table 1 ).
Classic TRALI
The Federal Drug Administration estimates that TRALI is the leading cause of transfusion-related deaths in the United States.[11,12] TRALI has been reported after transfusion of both blood and plasma containing blood components. Estimates of the incidence of TRALI include: 1 in 5000 units of packed RBC, 1 in 2000 plasma-containing components, and 1 in 400 units of whole-blood-derived platelet concentrates.[33-35] It is, however, likely that the true incidence of TRALI is much higher than reported, as it is likely that many cases have been misdiagnosed or confused with circulatory overload, cardiac failure, or as an anaphylactic type reaction. Indeed, a recent study reported TRALI in 8% of intensive care unit patients after the transfusion of a blood product.[36] Furthermore, it is likely that transfusion of blood products may cause mild pulmonary reactions that do not meet the strict definition of TRALI[37] and that the packed red cells and cryoprecipitate can cause TRALI suggests that small quantities of plasma (as little as 10% of a blood component unit) are sufficient to cause TRALI.
Two theories have been proposed to explain the pathophysiology of TRALI. The first suggests that an antibody-mediated reaction after transfusion of anti-granulocyte antibodies into patients who have leukocyte that express the cognate antigens is responsible for TRALI. The second postulates that TRALI is mediated by an interaction between biologically active mediators in banked blood products and the lung.[15,38,39] These two mechanisms of injury may not be mutually exclusive and a patient may develop TRALI through either one or both mechanisms. The antibody-mediated model postulates that the reaction is secondary to antibodies in donor plasma against antigens present on recipient leukocytes. These may be antibodies to the human leukocyte antigens (HLA) or other leukocyte antigens. HLA antibodies may be directed against either HLA class I antigens that are present in all leukocytes or HLA class II antigens that are found on B lymphocytes and monocytes. It has been suggested that most reactions are caused by antibodies in donor plasma and <10% of reactions are caused by plasma antibodies in the recipient that agglutinate the donor leukocytes. This antibody-antigen interaction can cause complement activation, resulting in the pulmonary sequestration and activation of neutrophils, endothelial cell damage, and a capillary leak syndrome in the lungs manifesting as TRALI.[19,38,40] There is evidence that TRALI is more common in recipients of blood products from multiparous female donors who are more likely to possess anti-HLA antibodies and anti-neutrophil-specific antibodies.[36,41] In an intriguing double-blind crossover study, Palfi et al.[42] randomized intensive care unit patients to receive plasma from multiparous female donors or those with no history of pregnancy or transfusion (control plasma). Transfusion of plasma from multiparous donors was associated with significantly lower oxygen saturation and higher tumor necrosis factor-in recipients than transfusion of control plasma.
In a sample of 308 randomly selected units of fresh frozen plasma, cryoprecipitate, platelets, and RBCs, 22% were positive for antileukocyte antibodies, 38% were directed against HLA class I antigens, 29% were directed against class II antigens, and 33% had both.[43] Cryoprecipitate and fresh frozen plasma had the highest rate of antibodies (24% and 29%, respectively), whereas RBCs had the lowest rate (17%). Given the high prevalence of antibodies in donated blood products, one would expect a relatively high rate of TRALI. However, this particular mechanism requires pairing of antigen-antibody among donor and recipient.
Various bioactive soluble mediators are released from stored white blood cells into human plasma during storage in a time dependent manner as the white blood cells deteriorate.[44] The concentrations of histamine, eosinophil cationic protein, eosinophilic protein X, myeloperoxidase, and plasminogen activator inhibitor-1 have all been reported to increase by 3-25-fold in the supernatant fluid of RBC components between day 0 and day 35 of storage.[45,46] In addition, stored red cells harbor potent pro-inflammatory cytokines such as interleukin (IL)-1, IL-6, IL-8, bactericidal permeability-increasing protein, phospholipase A2, and tumor necrosis factor, which increase in a time dependent manner with storage.[47,48] Prestorage leukocyte depletion has been shown to decrease the accumulation of these bioactive mediators.[47,49,50]
The biologically active mediator model postulates that TRALI is the result of two events.[51] The first event is the clinical condition of the patient, resulting in pulmonary endothelial activation and neutrophil sequestration, and the second event is the transfusion of biologically active mediators (lipids, cytokines) that activate adherent neutrophils leading to endothelial damage, capillary leak, and TRALI. The first event can be caused by a variety of insults to the pulmonary vascular endothelium such as sepsis, cardiopulmonary bypass, hematologic malignancy, thermal injury, and trauma. In an isolated rat lung model, ALI developed after the pulmonary vasculature was primed by lipopolysaccharide with subsequent infusion of supernatant from 42-day-old red cell concentrates.[52,53] ALI did not develop when fresh (day 0) red cell or platelet supernatants were used or when the tissue was not initially primed with lipopolysaccharide.[52,53]
Histologic findings in patients dying from TRALI are consistent with early ARDS, showing interstitial and intra-alveolar edema and an extravasation of neutrophils into the interstitial and air spaces.[34,54,55] More important, an increased number of neutrophils within the pulmonary capillary vasculature and small pulmonary vessels have been observed in lung sections from TRALI patients and a positive correlation between the degree of capillary leukostasis and the amount of proteinaceous fluid within the alveolar air spaces has been demonstrated.
When TRALI is suspected, the transfusion should be stopped immediately and the blood bank contacted to screen the donor unit(s) for antileukocyte antibodies. Serology demonstrating anti-HLA or anti-neutrophil-specific antibodies in donor blood is considered supporting evidence for the diagnosis of TRALI. Detection of a leukocyte antigen phenotype in the patient that matches the specificity of antibodies in the implicated donor further supports the diagnosis of TRALI.[19] Leukopenia is a common finding in patients with TRALI; both postulated pathogenic mechanism could explain this finding.[37] The treatment of TRALI is essentially supportive, i.e., a volume limited ventilatory strategy with scrupulous attention to the fluid balance.[56,57] In contrast to ALI/ARDS which has an associated mortality of approximately 40%, that of TRALI is estimated at between 5%-10%.[15,38,39]
Leukocyte reduction is controversial in transfusion medicine. Leukoreduction can be performed before storage or before transfusion. In terms of preventing classic TRALI, leukocyte reduction would appear to have a limited role, as the antibodies from the donor probably play a greater role than the leukocytes themselves. Leukodepletion may, however, reduce the incidence of delayed TRALI as leukocyte reduction has been demonstrated to reduce the accumulation of biologically active mediators in stored blood.[49,50] The study by Netzer et al.[58] supports this postulate. Furthermore, the length of blood storage before transfusion may affect the risk of developing delayed TRALI.
Delayed TRALI Syndrome
Transfusion of multiple units of RBCs has long been considered a risk factor for ALI.[21-23] Indeed, in the original description of ARDS by Ashbaugh et al.[59] in 1967, multiple blood transfusions were considered a risk factor in seven of the 12 patients described. Massive transfusion has been defined as transfusion of >10 units of RBC’s or whole blood within a 12-hr period or 15 units within a 24 hr period. The incidence of ARDS among those massively transfused patients may be as high as 57%.[27] Miller et al.[60] studied risk factors for developing ARDS in a cohort of 4,397 patients who sustained blunt trauma. In this study, the 24-hr transfusion of >10 packed red cells was an independent predictor for developing ARDS. Multiple transfusions have been reported to be the sole risk factor for ALI in up to 36% of multiply transfused patients.[61,62]
Although massive transfusion has long been identified as a risk factor for ALI/ARDS, transfusion of a smaller blood volume has until recently not been well studied and has not generally been considered a risk factor for ALI. However, several studies reported over the last 5 yrs have demonstrated that in intensive care unit patients with other risk factors for ALI, even a single unit of blood increases the risk for developing ALI/ARDS.[27-32] In these studies, the transfusion of blood or blood products was an independent risk factor for the development of ARDS with a pooled odds ratio (OR) of 2.13 (95% confidence interval, 1.75-2.52) (Figure 1).[64] We have coined the term delayed TRALI syndrome to describe ALI occurring in this setting. Patients who develop the delayed TRALI syndrome characteristically have additional risk factors for developing ALI, most notably sepsis, trauma, or burns.[27-32] The observation that blood transfusion increases the risk of ALI in critically ill patients is supported by the results from the Canadian Critical Care Trials Group study.[3] In this study, a liberal transfusion strategy was associated with an increased risk of ALI/ARDS (OR 1.5; 95% CI, 0.97-2.49). Similarly, Zilberberg et al.[32] observed that patients who received small numbers (<3 units) of packed red cell had an over two-fold increase in the risk for developing ARDS (OR 2.19; 95% CI 1.41-3.41) relative to patients receiving no transfusion. Boffard et al.[63] reported that both the transfusion requirements and incidence of ALI/ARDS (4% vs. 16%, p = 0.03) were significantly reduced in blunt trauma patients randomized to receive recombinant factor VII.
Figure 1.Effect of blood transfusions (any transfusion) on the risk of developing late transfusion-related acute lung injury (odds ratio and 95% confidence interval).[64] ICU, intensive care unit.
RBC transfusions may lead to delayed TRALI in up to 25% of transfused critically ill patients. This risk appears to increase with the number of units transfused to as high as 57% when 10 or more units of blood are transfused over a 24 hr period.[27,31,32] Furthermore, similar to classic TRALI, the risk of developing delayed TRALI is greater with transfusion of plasma-rich blood products, fresh frozen plasma, and platelets than transfusion with packed RBCs. In the study by Khan et al.[31] the odds ratio for developing delayed TRALI was 2.48 (95% CI, 1.29-4.74) in patients receiving fresh frozen plasma, 3.89 (95% CI, 1.36-11.52) in those receiving platelets, and 1.39 (95% CI, 0.79-2.43) in those who received RBC transfusions alone. The delayed TRALI syndrome may represent a phenomenon of immunomodulation caused by transfusions that renders the primed lung more vulnerable to ARDS (i.e., the two hit theory).[7,15,31] Further research needs to be done to elucidate the relationship of transfusion-related immunomodulation and the development of ARDS. Furthermore, the role of transfusion-related volume overload in exacerbating this syndrome requires investigation.
In addition to increasing the risk of developing ALI/ARDS, blood transfusions are associated with an increased risk of death in patients with established ARDS. Gong et al. and Netzer et al. have demonstrated that transfusion of RBCs in patients with established ALI/ARDS is an independent predictor of death.[30,58] In the study by Netzer et al., the risk of death was higher with the transfusion of nonleukodepleted as apposed to leukodepleted blood. The increased risk of death because of blood transfusion in patients with established ARDS is in keeping with the two hit model of TRALI. Presumably, the transfusion of primed white blood cells and proinflammatory mediators worsens the microvascular injury characteristic of ARDS.
Conclusions
ALI after transfusion can present as one of two syndromes; classic TRALI syndrome and delayed TRALI syndrome. Classic TRALI is characterized by the abrupt onset of respiratory failure within 2-6 hrs of transfusion of a blood product. It is usually caused by antileukocyte antibodies, resolves rapidly, and has a low mortality. A single unit of packed cells or blood component product is usually implicated. This is in contrast to the recently recognized delayed TRALI syndrome. The delayed TRALI syndrome occurs in up to 25% of critically ill patients receiving a blood transfusion, develops 6-72 hrs after the transfusion, and is associated with a mortality of up to 40%. The risk of delayed TRALI increases with increasing numbers of transfused blood products. The management of both the classic and delayed TRALI syndromes is essentially supportive and includes a volume limited ventilator strategy, prevention of volume overload and careful attention to the identification of and treatment of complicating pulmonary infections.
Table 1. Characteristics of Classic and Delayed TRALI Syndromes
![]()
References
|
Paul E. Marik, MD, FACP, FCCM, FCCP; E-mail: paul.marik@jefferson.edu .
![]()
1Division of Pulmonary and Critical Care Medicine, Thomas Jefferson University, Philadelphia, PA
2Section of Critical Care Medicine, Department of Anesthesiology, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Tags: News




Leave a Reply
You must be logged in to post a comment.