Margo A. Halm, RN, PhD, CNS-BC; Kathryn Krisko-Hagel, RN, MS
Am J Crit Care. 2008;17(5):469-472. ©2008 American Association of Critical-Care Nurses
Posted 10/28/2008
Introduction
Normal saline has been widely used in acute care settings during endotracheal and tracheostomy suctioning. Clinicians have held fast to this long-standing tradition because many were taught that normal saline breaks up secretions and aids in their removal (especially tenacious secretions). In this clinical review, we summarize current evidence related to the following questions: Does instilling normal saline during suctioning increase sputum yield? Alternatively, is this practice associated with adverse physiological and psychological effects?
Methods
The strategy included searching MEDLINE, CINAHL, Cochrane Library, Joanna Briggs Institute, and TRIP databases. Key words included endotracheal tubes, tracheostomies, normal saline, and suctioning. All types of evidence (nonexperimental, experimental, qualitative studies, systematic reviews) were included.
Results
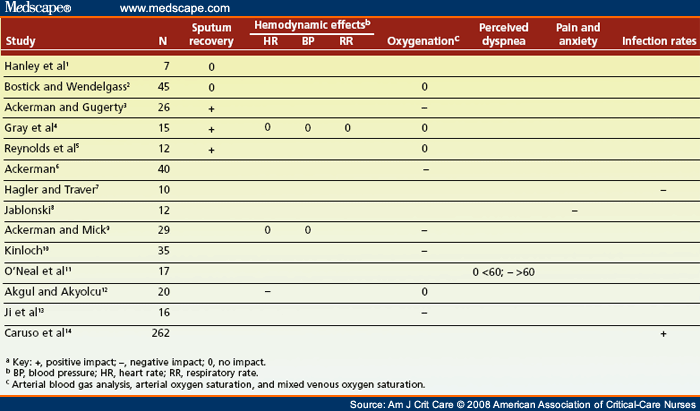
In the past 2 decades, investigators have studied the physiological and psychological effects of instillation of normal saline. The impact of the instillation of normal saline on sputum recovery, oxygenation, subjective symptoms, hemodynamic alterations, and infection was measured in 14 studies[1-14] ( Table 1 ). The effects of 2, 5, or 8 mL of normal saline on physiological parameters were evaluated at intervals of 5, 10, or 20 minutes (5 minutes most common). In one study,[1] researchers investigated saline deposition by radioactively labeling normal saline with technetium (Tc 99m). Samples included anesthetized dogs and ventilator-dependent patients in general, coronary artery bypass, and neurological intensive care units (ICUs). In addition to these studies, a guideline on tracheal suctioning from the Joanna Briggs Institute[15] was retrieved.
Sputum Recovery
Sputum volume or weight was measured in 5 of the 14 studies (36%).[1-5] In 3 of those 5 studies (60%), instillation of normal saline was associated with significantly increased retrieval of sputum. The difference in sputum volume ranged from 1 to 2 g, which may not be of clinical importance. In another study,[1] radioactively labeled normal saline was noted near the bottom of the endotracheal tube within 1 minute of instillation (rather than mixing with secretions) and was then rapidly absorbed by the cardiopulmonary system, providing evidence that normal saline and secretions do not mix. Furthermore, suctioning recovered a mean of only 18.7% of normal saline instilled in humans.
Oxygenation
Arterial blood gas analysis and measurement of the nadir and recovery time of oxygen saturation (most common) or mixed venous oxygen saturation were done in 9 studies.[2-6,9,10,12,13] Results of 56% of those studies indicated that use of normal saline was significantly associated with decreased oxygenation and desaturation that worsened over time after suctioning. Oxygen saturation was a mean of 1% to 2% lower when normal saline was used, which may, in itself, not be clinically significant. However, instillation of normal saline may impair gas exchange as evidenced by continued desaturation. More clinically impressive was the 6-point decrease in mixed venous oxygen saturation that Kinloch[10] observed in patients suctioned 5 minutes after instillation of normal saline (compared with controls), as well as the doubled recovery time. These findings demonstrate the detrimental effect of normal saline on global tissue oxygenation.
Subjective Symptoms: Pain, Anxiety, Dyspnea
Subjective symptoms associated with instillation of normal saline were explored in 2 studies[8,11] (14%). Exploring the experience of being suctioned with normal saline, Jablonski[8] found that patients reported anxiety and dread, as well as increased pain. In another study, O’Neal et al[11] found increased perceived dyspnea in patients over age 60 that persisted for up to 10 minutes after suctioning, a finding that may be related to decreased pulmonary compliance with aging.
Hemodynamic Alterations
Hemodynamic effects were investigated in 3 studies[4,9,12] (21%). Results of 1 of these studies[12] demonstrated that instillation of normal saline was associated with increased heart rate 4 to 5 minutes after suctioning; however, no effect on blood pressure or respiratory rate was uncovered. The increased stimulation of the cough reflex associated with instillation of normal saline may have other detrimental effects such as increased mean arterial pressure and intracranial pressure.[15,16]
Infection
Risk of infection was investigated in 2 studies[7,14] (14%). Hagler and Traver[7] found sputum cultures that showed growth due to the dislodgment of bacterial colonies. Up to 5 times as many colonies were dislodged when normal saline was instilled, and therefore this practice may contribute significantly to lower airway contamination. Newer evidence from a randomized controlled trial[14] suggests that instillation of normal saline was associated with a lower incidence of ventilator-associated pneumonia. It is unclear from this abstract whether the researchers controlled for other standard interventions to avoid ventilator-associated pneumonia[17,18] such as oral care, aspiration of subglottic secretions, maintenance of cuff pressure on the endotracheal tube, and prophylaxis of peptic ulcer and deep vein thrombosis.
Recommendation Based on Current Evidence
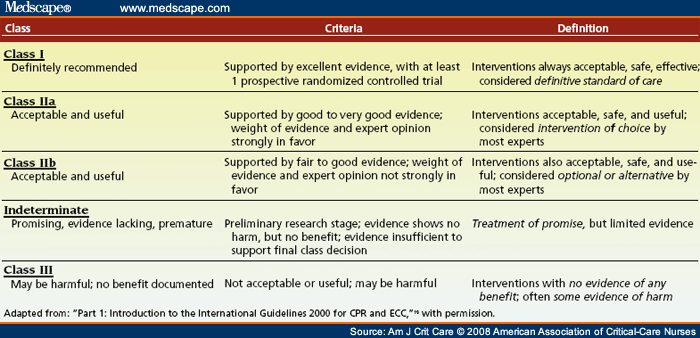
Collectively, these studies provide class III evidence of the adverse physiological and psychological effects of instillation of normal saline, and therefore, support against the routine use of normal saline with suctioning ( Table 2 ). Normal saline and mucus do not mix. Therefore, normal saline does not thin or mobilize secretions. Rather, ensuring adequate hydration is one way that nurses can facilitate removal of secretions.[15] The best-known interventions for managing thick tenacious secretions and preventing mucus plugs in ventilator-dependent patients are hydration, adequate humidification, use of mucolytic agents, and effective mobilization.[16,18,20]
In addition to an unappreciable increase in sputum recovery, use of normal saline adversely affects arterial and global tissue oxygenation and dislodges bacterial colonies, thus contributing to lower airway contamination. Because no solid scientifically based benefits for routine use of normal saline have been shown, it is highly recommended that this potentially harmful “sacred cow” be abandoned. Instead, treatment considerations should center on ways to prevent the development of thick, tenacious secretions.[20]
Normal saline may be indicated in situations where it is necessary to elicit a cough,[4,18] and normal saline may be useful for clearing the catheter after suctioning to avoid reintroducing pathogens into the airway.[21] Good handwashing is essential to reduce infection when opening vials of normal saline because increased contamination has been documented when clinicians use the nongloved thumb to twist off the tops of the vials.[22]
Despite these recommendations, organizational change toward best suctioning practices has not been without challenges. In a recent multisite study,[23] three large institutions had policies that recommended instilling normal saline for thick secretions. Suctioning surveys[23,24] also indicate that 2 to 3 times as many respiratory therapists as nurses report continued use of normal saline—a finding that is not so surprising given that the American Association of Respiratory Care’s guideline[25] has not been updated since 1993 (and still advocates that normal saline dilutes and mobilizes secretions).
Promisingly, among nursing circles, researchers in the United Kingdom reported that although observed suctioning practices were contrary to many research recommendations,[26] educational interventions proved effective in advancing the knowledge and translation of research-based suctioning practices of critical care nurses at the bedside.[27]
Others have also reported high compliance rates of nurses with evidence-based guidelines recommending avoidance of normal saline.[28] More studies are needed to document clinical adherence to evidence-based guidelines so that we can better connect processes of care to outcomes for patients.
Table 1. Evidence Summary of Studies on Instilling Normal Saline During Suctioninga
Table 2. Levels of Evidence
![]()
References
|
The authors acknowledge the work of the 2004 United Nursing Research Council (Miriam Blalock, Becky Braden, Lisa Chute, Norbert Erben, Anna Gryczman, Dave Larson, Diane Lemay, Julie Sabo, Laura Senn, Bette Sisler, Linda Strom, Deb Topham, and Jen Wells) in reviewing studies related to the use of normal saline during suctioning.
Corresponding author: Margo A. Halm, RN, PhD, CNS-BC, United Hospital -Mailstop 60231, 333 N. Smith Ave, St Paul, MN 55102 (e-mail: margo.a.halm@allina.com ).
To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 809-2273 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org .
![]()
Margo A. Halm, is a clinical nurse specialist and director of nursing research and quality at United Hospital in St Paul, Minnesota, where she leads and mentors staff in principles of clinical research and evidence-based practice.
Kathryn Krisko-Hage, is a learning and development specialist at United Hospital in St Paul, Minnesota.
Tags: News




Leave a Reply
You must be logged in to post a comment.