Updated: Aug 11, 2010
Introduction
Blocking the pudendal nerve with injection of local anesthetic is used for vaginal deliveries and for minor surgeries of the vagina and perineum. Use of this nerve block for vaginal delivery was reported as early as 1916.[1 ]However, the procedure did not become popular until 1953-54, when Klink and Kohl implemented the modified technique.[2,3 ]
The sensory and motor innervation of the perineum is derived from the pudendal nerve, which is composed of the anterior primary divisions of the second, third, and fourth sacral nerves. The pudendal nerve’s 3 branches include the following:
- Dorsal nerve of clitoris, which innervates the clitoris
- Perineal branch, which innervates the muscles of the perineum, the skin of the labia majora and labia minora, and the vestibule
- Inferior hemorrhoidal nerve, which innervates the external anal sphincter and the perianal skin
A pudendal nerve block targets the pudendal nerve trunk as it enters the lesser sciatic foramen, about 1 cm inferior and medial to the attachment of the sacrospinous ligament to the ischial spine. Here, the nerve is medial to the internal pudendal vessels. This nerve is accessed by 2 approaches, transvaginal and transcutaneous (or perineal). The former approach is more reliable and is used most often, except when an engaged head makes vaginal palpation more difficult. The anatomical basis for both approaches is to block the nerve proximal to its terminal branches.
Indications
While neuroaxial analgesia continues to replace pudendal nerve block as the technique of choice, there are and will always remain situations in which anesthesia service is unavailable. In this event, pudendal block provides a suitable alternative for the following:
- Analgesia for the second stage of labor
- Repair of an episiotomy or perineal laceration
- Outlet instrument delivery (to assist with pelvic floor relaxation)
- Used in the past as an alternative to neuroaxial analgesia in assisted twin and breech deliveries
- Minor surgeries of the lower vagina and perineum
Contraindications
- Patient refusal
- Patient’s inability to cooperate
- Patient sensitivity to local anesthetics
- Presence of infection in the ischiorectal space or the adjacent structures, including the vagina or perineum
- Coagulation disorders
Anesthesia
- Lidocaine 1% is often used for pudendal nerve block. Agents that could be used instead include 2-chloroprocaine 2%, bupivacaine 0.25%, prilocaine 1%, or mepivacaine 1%.
- Because of its short duration of action, 2-chloroprocaine 2% is used less often. However, its rapid onset of action provides an advantage if the block is performed immediately before delivery. Another advantage of 2-chloroprocaine 2% comes from its rapid metabolism and short intravascular half-life, which decrease the risk of maternal and fetal toxicity.
- Studies by Kuhnert et al show no clinically significant difference in the neonatal neurobehavior at 4 h and 24 h after delivery, regardless of the type of anesthetic used.[6 ]
- Although some obstetricians contend that the addition of epinephrine to the local anesthetic solution improves the quality of the block, Schierup et al failed to demonstrate such improvement in the quality of anesthesia in their study of adding epinephrine to mepivacaine.[7 ]Interestingly, the addition of epinephrine slightly prolonged the interval between the block administration and delivery. Maternal venous blood mepivacaine concentrations were slightly higher in the group without epinephrine, but no such differences were noted in umbilical cord blood samples.
Equipment
- Iowa trumpet or similar guide (eg, Kobak) to facilitate the placement of the needle (see image below)
-
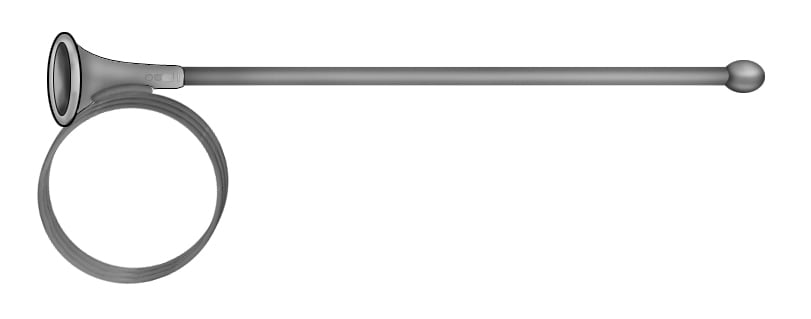
Iowa trumpet.
- Needle, usually 6 in, 20-22 gauge (ga)
- Syringe with finger ring, 10 mL
- Local anesthetics (eg, lidocaine 1%)
- Sterile gloves
- Resuscitation equipment and medications in case an adverse reaction to the anesthetic is encountered
Positioning
- The block is performed with the patient in the lithotomy position.
Technique
- Usually, no vaginal preparation is needed.
- Palpate the ischial spine. This is usually done transvaginally but can also be done through the rectum.
- Be sure to use a needle with a guide (either the Iowa trumpet or the Kobak needle guide) to limit the depth of submucosal penetration and to prevent injury to the vagina and the fetus.
- To perform a left-sided block, palpate the ischial spine with the index finger of the left hand, hold the syringe in the right hand, and guide the needle between the index and middle finger of the left hand toward the ischial spine.
- The authors the following 3-injection technique:
- Place the end of the guide beneath the tip of the ischial spine.
- Push the needle into the vaginal mucosa.
- Aspirate to ensure that the injection is not intravascular.
- Raise a mucosal wheal with 1 mL of local anesthetic.
- Advance the needle through the vaginal mucosa until it touches the sacrospinous ligament 1 cm medial and posterior to the ischial spine.
- Infiltrate the tissue with 3 mL of local anesthetic.
- Next, advance the needle further through the sacrospinous ligament for a distance of 1 cm until a loss of resistance is appreciated.
- The tip now lies in the area of the pudendal nerve. At this point, the pudendal vessels lie just lateral to the pudendal nerve, so care must be taken to avoid intravascular administration. Aspirate to confirm the needle placement is not intravascular prior to injecting lidocaine.
- Inject another 3 mL of local anesthetic solution into this region.
- Subsequently, withdraw the needle into the guide and move the tip of the guide to just above the ischial spine.
- At this new location, reinsert the needle though the mucosa and again inject 3 mL of local anesthetic.
- Many practitioners use a single 10-mL injection instead of the 3-injection technique described above. The single injection is done after the needle is introduced nearly 1 cm through the sacrospinous ligament medial and posterior to the ischial spine.
- To block the right side of the pelvis, repeat these steps using the right hand to hold the needle and needle guide (see image below).
-
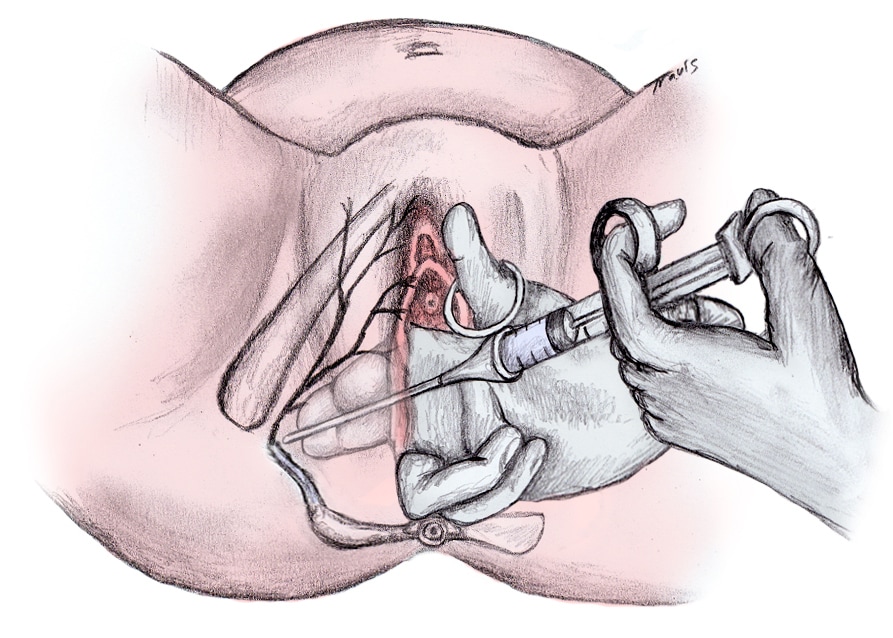
Pudendal block, transvaginal approach.
- This block could be attempted under ultrasonographic, CT, or fluoroscopic guidance. Although imaging helps delineate the anatomic landmark for needle placement, it is rarely used by obstetricians and gynecologists.
Additional anesthesia
- Even in the best hands, pudendal anesthesia is less than 100% reliable. The patient must be checked bilaterally for loss of anal wink reflex before proceeding with the surgical procedure. If mild stimulus does not elicit a reflex response, a pinch confirms the effectiveness of bilateral anesthesia.
- A smaller repeat dose can be used if an adequate block is not seen, but care must be taken to avoid toxic serum levels.
- Appropriate monitoring of the patient and the fetus is mandatory, and intravenous access should be readily available. Provisions should be made for rapid resuscitation should toxicity or adverse reactions occur.
- Keep in mind that the pudendal block provides inadequate anesthesia for mid-forceps delivery, deliveries that require uterine manipulation, postpartum examination and repair of the upper vagina and cervix, and manual exploration of the uterine cavity.[4 ]
- Under these circumstances, the addition of intravenous narcotics may provide appreciable, though not total, relief from pain.
- With such an approach, caution must be exercised to avoid dosages or combinations of narcotics and sedatives that might obtund the patient and cause possible airway obstruction or aspiration.
Timing of procedure
- Timing of block placement is important, since at least 5-10 minutes are required for the infiltration to take effect.
- Most US obstetricians perform pudendal block immediately prior to delivery. This practice reflects the concern that perineal anesthesia may prolong the second stage of labor.
- Anesthesia may last 20-60 minutes, depending on the agent used with or without epinephrine.
- In patients without neuroaxial analgesia, the pudendal block can be performed when the patient reports vaginal or perineal pain.
- With early pudendal nerve block, the obstetrician may repeat the block, if necessary, so long as the maximum dose of local anesthetic is not exceeded.
Efficacy
- Efficacy varies depending on the experience of the obstetrician.
- Unilateral or bilateral failure is common, with success rates of only 50% with the transvaginal route and approximately 25% with the transperineal route.[5 ]
- Obstetricians typically perform simultaneous perineal infiltration, especially if the block was not placed until just prior to delivery. If delivery occurs before the pudendal block has become effective, an episiotomy can still be made without pain. By the time of the repair, the pudendal block usually has become effective.
Pearls
- Pudendal nerve block does not abolish sensation to the anterior part of the perineum, as the perineum is supplied by branches of the ilioinguinal and genitofemoral nerves.
- Failure to wait a sufficient time after injection is a common reason for block failure.
- Pudendal block does not abolish the pain of uterine contractions and cervical dilatation; this sensation is transmitted by the sympathetic fibers derived from the spinal levels of T10-L2.
- This block does not help relax the uterus.
- The obstetrician should be alert to the total dose of local anesthetic given, especially in cases of repetitive pudendal nerve blocks or pudendal nerve block in association with perineal infiltration. When lidocaine without epinephrine is used, the dose recommended is 4.5 mg/kg. When lidocaine with epinephrine is used, the recommended dose is 7 mg/kg. The maximum dose of lidocaine used should not exceed 300 mg. When bupivacaine without epinephrine is used, the recommended dose is 2.5 mg/kg, with the maximum dose not to exceed 175 mg. When used with epinephrine, the maximum dose of bupivacaine that could be used is up to 225 mg.
- Be sure to use a needle with a guide (either the Iowa trumpet or the Kobak needle guide) to limit the depth of submucosal penetration and to prevent injury to the vagina and the fetus.
Complications
Potential complications should be explained to the patient prior to getting informed consent. These complications are uncommon but may be serious. Direct intravascular injections or systemic absorption of an excessive dose of local anesthetic may result in systemic toxicities. Other risks include the following:
- Laceration of the vaginal mucosa is a potential complication.
- The second stage of labor may be prolonged[8 ]due to a loss of the bearing-down reflex, particularly when local anesthetics are combined with epinephrine (does not affect incidence of instrument delivery).[9 ]
- Systemic anesthetic complications, though rare and usually transient, may include palpitation, tinnitus, dysarthria, drowsiness, confusion, loss of consciousness, convulsions, hypotension, and bradycardia.
- Hematomas (vaginal, retroperitoneal, and ischiorectal) from injury to the pudendal artery can be a complication of pudendal block, particularly with defective coagulation.[10 ]Hematomas are usually small, and surgical intervention is rarely needed.
- Infection (retro psoas and subgluteal abscess) has occasionally been reported, spreading superiorly along the psoas muscle or laterally along the obturator internus. Infrequent occurrence and diagnostic difficulties make these abscesses especially dangerous.[11,12,13 ]Maintain a high suspicion for infection when severe pain in the back or hip, limitation of motion, and, especially, increasing fever follow pudendal anesthesia prior to vaginal delivery.
- Ischial region paresthesia on the first postpartum day,[9 ]or sacral neuropathy, may occur.
- Needle-stick injury with associated risk of exposure to HIV and other bloodborne diseases may result, as the needle guide does not uniformly protect the physician and the procedure requires multiple blind needle punctures.
- Fetal complications are uncommon but may result from fetal trauma and or direct fetal injection of local anesthetic.[14,15 ]Possible intoxication by local anesthetics should be considered when neonatal distress is seen at birth following the use of pudendal block. Typical features include hypotonia, papillary mydriasis fixed to light, apnea, and seizures. Complete recovery usually occurs.
Multimedia
Media file 1: Iowa trumpet.
Media file 2: Pudendal block, transvaginal approach.
References
- King R. Perineal anesthesia in labor. Surg Gynecol Obstet. 1916;23:615-8.
- Klink EW. Perineal nerve block; an anatomic and clinical study in the female. Obstet Gynecol. Feb 1953;1(2):137-46. [Medline].
- Kohl GC. New method of pudendal block. Northwest Med. Oct 1954;53(10):1012-3. [Medline].
- Hutchins CJ. Spinal analgesia for instrumental delivery. A comparison with pudendal nerve block. Anaesthesia. Apr 1980;35(4):376-7. [Medline].
- Scudamore JH, Yates MJ. Pudendal block–a misnomer?. Lancet. Jan 1 1966;1(7427):23-4. [Medline].
- Kuhnert BR, Knapp DR, Kuhnert PM, Prochaska AL. Maternal, fetal, and neonatal metabolism of lidocaine. Clin Pharmacol Ther. Aug 1979;26(2):213-20. [Medline].
- Schierup L, Schmidt JF, Torp Jensen A, Rye BA. Pudendal block in vaginal deliveries. Mepivacaine with and without epinephrine. Acta Obstet Gynecol Scand. 1988;67(3):195-7. [Medline].
- Zador G, Lindmark G, Nilsson BA. Pudendal block in normal vaginal deliveries. Clinical efficacy, lidocaine concentrations in maternal and foetal blood, foetal and maternal acid-base values and influence on uterine activity. Acta Obstet Gynecol Scand Suppl. 1974;51-64. [Medline].
- Langhoff-Roos J, Lindmark G. Analgesia and maternal side effects of pudendal block at delivery. A comparison of three local anesthetics. Acta Obstet Gynecol Scand. 1985;64(3):269-72. [Medline].
- Kurzel RB, Au AH, Rooholamini SA. Retroperitoneal hematoma as a complication of pudendal block. Diagnosis made by computed tomography. West J Med. Jun 1996;164(6):523-5. [Medline].
- Wenger DR, Gitchell RG. Severe infections following pudendal block anesthesia: need for orthopaedic awareness. J Bone Joint Surg Am. Jan 1973;55(1):202-7. [Medline].
- Hibbard LT, Snyder EN, McVann RM. Subgluteal and retropsoal infection in obstetric practice. Obstet Gynecol. Jan 1972;39(1):137-50. [Medline].
- Svancarek W, Chirino O, Schaefer G Jr, Blythe JG. Retropsoas and subgluteal abscesses following paracervical and pudendal anesthesia. JAMA. Feb 28 1977;237(9):892-4. [Medline].
- Schnider SM, Levinson G, Ralston DH. Regional anesthesia for labor and delivery. In: Schnider SM, Levinson G, editors. Anesthesia for Obstetrics. 3rd Edition. Baltimore: Williams & Wilkins; 1993:135-153.
- Chase D, Brady JP. Ventricular tachycardia in a neonate with mepivacaine toxicity. J Pediatr. Jan 1977;90(1):127-9. [Medline].
Keywords
transvaginal pudendal block, pudendal nerve, pudendal nerve block, transvaginal pudendal nerve block, transvaginal nerve block, labor anesthesia, pudendal anesthesia, perineal anesthesia, episiotomy, episiotomy repair, pudendal repair, transvaginal approach, transcutaneous approach, perineal approach, local anesthesia, vaginal delivery anesthesia, vaginal anesthesia, perineum anesthesia, perineum nerve block, dorsal nerve of clitoris, inferior hemorrhoidal nerve
Contributor Information and Disclosures
Author
Hemant K Satpathy, MD, Fellow, Division of Maternal-Fetal Medicine, Emory School of Medicine
Hemant K Satpathy, MD is a member of the following medical societies: American Association of Gynecologic Laparoscopists, American College of Obstetricians and Gynecologists, American Medical Association, and Society for Maternal-Fetal Medicine
Disclosure: Nothing to disclose.
Coauthor(s)
Donald R Frey, MD, Associate Professor, Department of Family Medicine, Dr Roland L Kleeberger Endowed Chair, Creighton University School of Medicine; Chief, Family Medicine Service, Creighton University Medical Center; Medical Director, St Joseph Villa Skilled Nursing Facility
Donald R Frey, MD is a member of the following medical societies: American Academy of Family Physicians, American Geriatrics Society, American Public Health Association, and Society of Teachers of Family Medicine
Disclosure: Nothing to disclose.
Alfred D Fleming, MD, FACOG, Associate Professor of Obstetrics and Gynecology, Associate Professor, Department of Radiology, Chairman, Department of Obstetrics and Gynecology, Assistant Dean for Clinical Medical Education, Creighton University School of Medicine; Co-director of Perinatal Ultrasound, Department of Obstetrics and Gynecology, Creighton University Medical Center
Alfred D Fleming, MD, FACOG is a member of the following medical societies: American College of Obstetricians and Gynecologists
Disclosure: Nothing to disclose.
Katie A Fossen, MD, Residency in Obstetrics and Gynecology, Creighton University School of Medicine Affiliated Hospitals
Katie A Fossen, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Obstetricians and Gynecologists, American College of Physicians, American Medical Association, American Medical Student Association/Foundation, and American Medical Women’s Association
Disclosure: Nothing to disclose.
Medical Editor
Alex Macario, MD, MBA, Professor of Anesthesia, Program Director, Anesthesia Residency, Professor (Courtesy), Department of Health Research and Policy, Stanford University School of Medicine
Alex Macario, MD, MBA is a member of the following medical societies: American Medical Association, American Society of Anesthesiologists, California Medical Association, and International Anesthesia Research Society
Disclosure: Nothing to disclose.
Pharmacy Editor
Mary L Windle, PharmD, Adjunct Associate Professor, University of Nebraska Medical Center College of Pharmacy; Pharmacy Editor, eMedicine
Disclosure: Nothing to disclose.
Chief Editor
David Chelmow, MD, Professor and Chair, Department of Obstetrics and Gynecology, Virginia Commonwealth University School of Medicine
David Chelmow, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists, American Medical Association, Association of Professors of Gynecology and Obstetrics, Massachusetts Medical Society, Phi Beta Kappa, Sigma Xi, Society for Gynecologic Investigation, and Society for Medical Decision Making
Disclosure: Nothing to disclose.
I appreciate the support of my wife, Jayashree, and my parents.
Further Reading
© 1994-2010 by Medscape.
All Rights Reserved
(http://www.medscape.com/public/copyright)
Tags: Anestesia




One Response to “Transvaginal Pudendal Nerve Block”
Trackbacks/Pingbacks
Leave a Reply
You must be logged in to post a comment.