William V. Harford, MD; Corinne Glynn, MD; J. Esteban Varela, MD; Ali A. Siddiqui, MD
Rectovesical fistulas may be present in patients with primary and recurrent rectal tumors.[1] In patients with inoperable rectal cancer and a rectovesicular fistula, palliative surgical therapy includes a diverting colostomy. Palliation after these procedures is often only partial, with the development of recurrent infections and stoma problems.[2] We describe what we believe to be the second reported case in the literature of a rectovesical fistula that was effectively treated with a covered self-expanding metal stent (SEMS).[3]
Case Report
A 66-year-old man with a history of metastatic rectal carcinoma was admitted due to fecaluria, increasing constipation, and abdominal pain. A computed tomographic (CT) scan with contrast enema showed a 5-cm near-occlusive malignant stricture in proximal rectum with a fistula to the urinary bladder (Figure 1). Performance of diverting colostomy was not recommended given his high operative risk. Insertion of a covered SEMS across the malignant stricture was considered to palliate both the obstructive symptoms and relieve the fecaluria.

Figure 1.Image obtained after administration of contrast enema showing contrast within the urinary bladder compatible with a rectovesicular fistula (see arrow).
A lower endoscopy revealed a circumferential proximal rectal mass causing almost complete luminal obstruction (Figure 2). Gastrografin was introduced into the rectum via a sclerotherapy injection catheter, and 5-cm rectal stricture was identified. Under fluoroscopic guidance, a flexible 0.035-in guide wire (Jagwire, Boston Scientific, Natick, Massachusetts) was advanced through the stenosis. The malignant stricture was dilated with a 15-mm-outside diameter dilation balloon. Subsequently, a covered esophageal SEMS (Alveolus, Charlotte, North Carolina), 9 cm long and 22 mm in diameter, was successfully deployed across the rectal stricture under fluoroscopic guidance (Figure 3). A copious amount of liquid stool ensued after the deployment. An abdominal film confirmed the position of the stent.

Figure 2.Circumferential ulcerated rectal mass causing almost complete luminal obstruction.
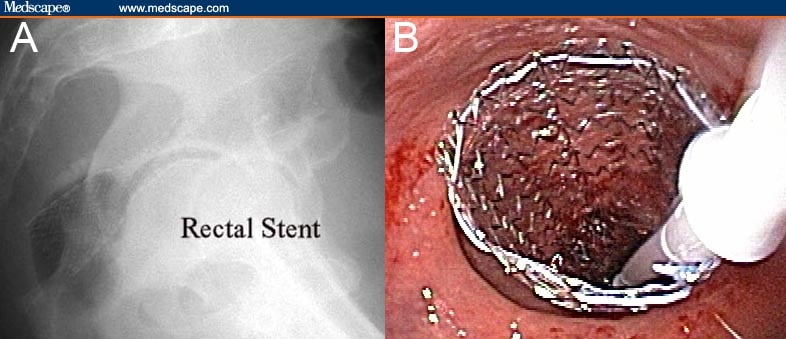
Figure 3.Self-expanding metal stent: A. X-ray showing successful deployment of SEMS across rectal mass. B. Endoscopic view of SEMS deployed across rectal mass.
Fecaluria stopped immediately afterward, and a repeat CT scan did not reveal any further evidence of the fistula. During the observation period, the patient remained asymptomatic and was discharged home. The patient continued to do well at home, and a follow-up barium study 1 month later revealed good position of the rectal stent and no evidence of a rectovesicular fistula, with complete obliteration of the fistulous tract. The patient died uneventfully 2 months later. The family refused an autopsy.
Discussion
Patients with inoperable colorectal cancer who develop a rectovesicular fistula are usually referred for a palliative diverting colostomy. However, diverting colostomy is a morbid procedure with recurrent infections and a stomal complication rate up to 36%.[4,5]
Insertion of SEMS in the rectum is a simple procedure for palliative treatment of malignant strictures in patients with inoperable rectal cancer.[6-10] We propose that SEMS can also be used as a nonoperative alternative to a diverting colostomy for palliation of rectovesicular fistula from advanced cancer.
For adequate closure of the rectovesical fistula, it is imperative that we use SEMS with an external membranous covering. However, there are no commercially available membrane-covered SEMS for use in the bowel; hence, we used a polyurethane-covered esophageal SEMS. The SEMS recanalized the strictured portion of the rectum to maintain luminal patency. The rectovesical fistula was closed due to compression of the tissue by the polyurethane membrane covering the stent. The palliative function of the stent was good during the observation time.
Closure of a bowel fistula by inserting a covered stent is particularly useful in patients who are unfit for surgery at the time of presentation and may benefit from a nonoperative approach to resolve their symptoms.[8,9] The high technical success rate of stent deployment (82% to 100%) coupled with a low complication rate (< 10%) argues favorably for following this nonsurgical approach.[10,11] The most common complication of colorectal stenting is stent obstruction caused by tumor-related ingrowth or overgrowth or by impaction of feces. Tumor ingrowth obstructions can be managed by ablation of the obstruction or by placement of a second stent. For tumor overgrowth, placement of a second stent is effective.
In summary, palliative stent placement for a rectovesicular fistula in unresectable obstructive colon cancer is a safe and effective procedure. This procedure allows patients with unresectable colorectal cancers to avoid more invasive surgical treatment and gain enhanced quality of life.[12]
Reader Comments on: Palliation of a Malignant Rectal Stricture and Rectovesical Fistula With Colonic Stenting
See reader comments on this article and provide your own.
Readers are encouraged to respond to the author at ali.siddiqui@utsw.edu or to Peter Yellowlees, MD, Deputy Editor of The Medscape Journal of Medicine, for the editor’s eyes only or for possible publication as an actual Letter in the Medscape Journal via email: peter.yellowlees@ucdmc.ucdavis.edu
References
|
![]()
Corinne Glynn, MD, University of Iowa, Iowa City, Iowa
J. Esteban Varela, MD, Assistant Professor, Department of Surgery, Dallas Veterans Affairs Medical Center, University of Texas Southwestern Medical School, Dallas, Texas
Ali A. Siddiqui, MD, Assistant Professor of Medicine, Division of Gastroenterology, Dallas Veterans Affairs Medical Center, University of Texas Southwestern Medical School, Dallas, Texas
Author’s email: ali.siddiqui@utsw.edu
Disclosure: Corinne Glynn, MD, has disclosed no relevant financial relationships in addition to her employment.
Disclosure: J. Esteban Varela, MD, has disclosed no relevant financial relationships in addition to his employment.
Disclosure: Ali A. Siddiqui, MD, has disclosed no relevant financial relationships in addition to his employment.
Tags: News




Leave a Reply
You must be logged in to post a comment.